In news– Recently a new target was found to combat AMR Salmonella.
What does the new study say?-
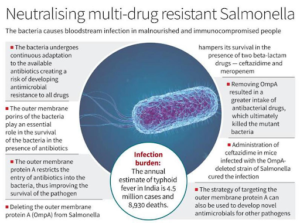
- A recent study carried out by our group showed that outer membrane porins of Salmonella Typhimurium play an essential role in the survival of the bacteria in the presence of antibiotics.
- In this study, scientists showed that deleting outer membrane protein A (OmpA) from Salmonella hampered its survival in the presence of two β-lactam drugs — ceftazidime and meropenem.
- OmpA is one of the most abundant barrel-shaped porin proteins localised in the outer membrane of Salmonella.
- The absence of OmpA in Salmonella hampers the stability of the bacterial outer membrane and reduces the expression of efflux pump genes.
- The study further showed that the outer membrane protein A could restrict the entry of antibiotics into the bacteria, thus improving the survival of the pathogen under antibiotic treatment.
- Removing OmpA resulted in a greater intake of ceftazidime and meropenem, which ultimately killed the mutant bacteria by disrupting its outer envelope.
- Most importantly, this study showed that disruption of OmpA can also effectively reduce the antibiotic-resistant persister population of Salmonella.
- The loss of integrity of the bacterial outer membrane in the absence of OmpA made the bacteria highly susceptible to killing by the host’s innate immune system.
- Other Gram-negative pathogens ( Escherichia coli, Acinetobacter baumannii, Klebsiella pneumoniae, Pseudomonas aeruginosa, etc.) use outer membrane porins for various purposes, ranging from maintaining outer membrane stability to developing antimicrobial resistance.
- As demonstrated in the study, the strategy to target outer membrane protein A (OmpA) of Salmonella can also be used to develop novel antimicrobials for other pathogens that can effectively reduce the risk of antimicrobial resistance (AMR) in the future.
AMR Salmonella & its threat-
- The rapid and unselective use of traditional antibiotics gives rise to the emergence of drug resistant phenotype in typhoidal and non-typhoidal Salmonella serovars, which has increased the difficulties in curing Salmonella-induced food-borne illnesses (majorly typhoid or paratyphoid fever, gastroenteritis, and diarrhoea) worldwide.
- Salmonella typhimurium ST313, an invasive non-typhoidal Salmonella serovar, causes bloodstream infection in the malnourished and immunocompromised population of sub-Saharan Africa.
- Recent studies have reported the emergence of multi-drug resistant (MDR) phenotype in Salmonella tphimurium DT104, which causes infection in humans and cattle.
- The MDR phenotype in this pathogen was provided by Salmonella Genomic Island-1 (SGI-1), which confers protection against a wide range of antibiotics, including ampicillin (pse-1), chloramphenicol/florfenicol (floR), streptomycin/spectinomycin (aadA2), sulphonamides (sul1), and tetracycline (tetG) (ACSSuT).
- Further emergence of extensively drug-resistant (XDR) S. Typhimurium ST313 (having multi-drug resistant (MDR) and resistance against extended-spectrum beta-lactamase and azithromycin) in Africa posed a significant threat to global health.
- Recent studies reported an annual incidence of as many as 360 cases of typhoid fever per 1,00,000 people with 8,930 deaths (0.2% fatality rate) in India.
- The continuous adaptation of this bacteria to the available antibiotics creates a risk of developing antimicrobial resistance in the future.